What is Blood Cancer?
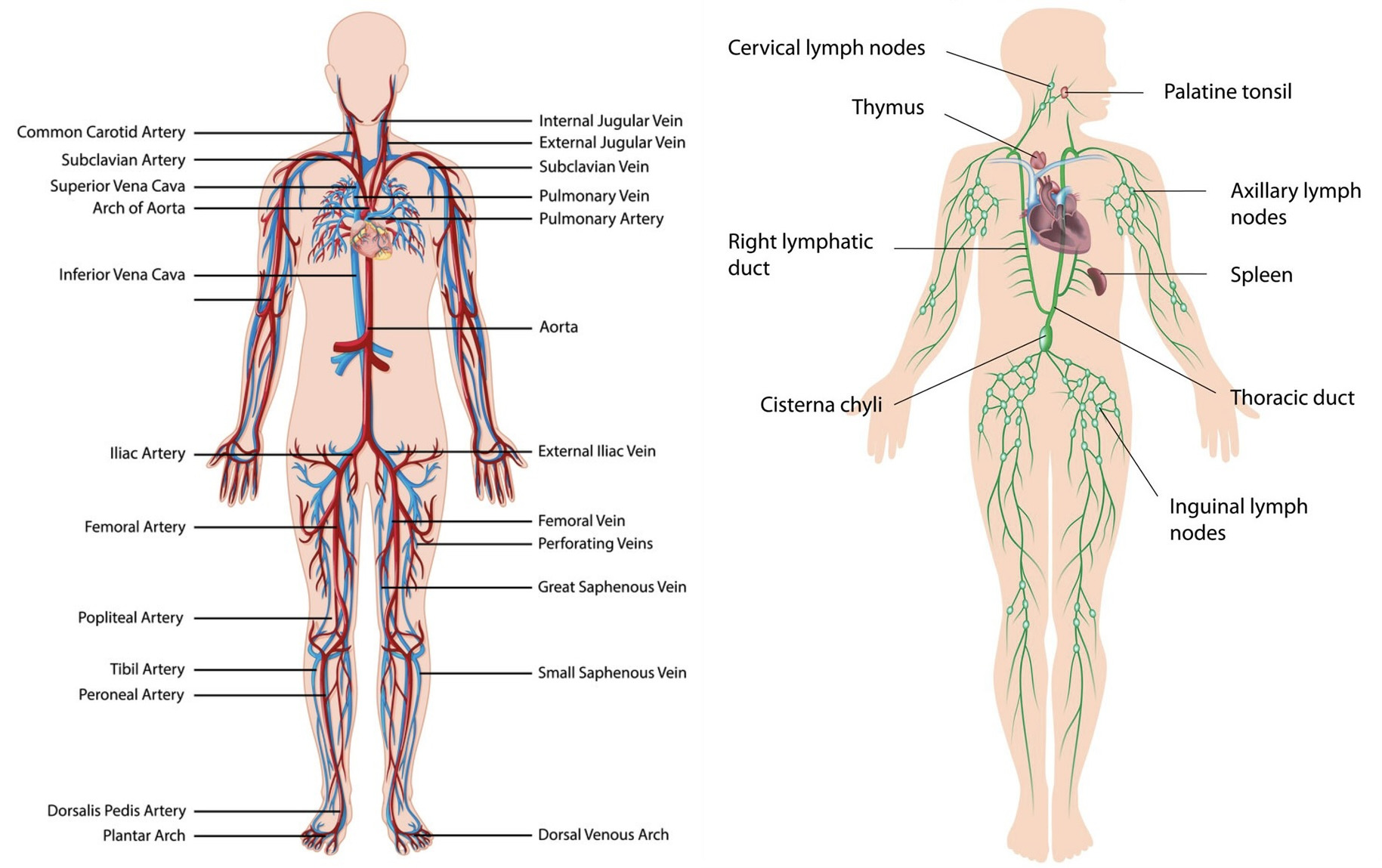
Blood cancers affect blood cells. Cancer can affect red blood cells (RBCs) that carry oxygen throughout your body, and platelets help your blood clot. Furthermore, there are also types of cancers that affect the lymphatic system. Consequently, the lymphatic system is responsible for White Blood Cells (WBCs), which are critical in fighting disease and infection.
Therefore, when someone has any type of blood cancer, their cells grow and divide rapidly, inhibiting the blood’s necessary functions. For example, your blood might not clot if you scrape your knee, or if you get sick, your body will have a weakened immune system to fight the illness.
Types of Blood Cancer:
The disease has various forms, and each type is further categorized. Below are the most common types:
- Leukemia – Affects the bone marrow and WBC.
- Lymphoma – Affects the lymphatic glands.
- Myeloma – Affects plasma cells.
- Myelodysplastic syndromes (MDS) – Affects the bone marrow. It is also known as Bone Marrow Failure.
Ireland Blood Cancer Statistics:
- Doctors diagnose approximately 485 people with a form of leukemia each year.
- Doctors diagnose approximately 1000 people with a form of lymphoma each year.
- Doctors diagnose approximately 380 people with a form of Myeloma each year.
- Doctors diagnose approximately 175 people with a form of MDS each year.
- Lymphoma is the 5th most common type of cancer diagnosed in men and children.
- Leukemia is the most common type of cancer diagnosed in children.
Signs and Symptoms:
Each form of blood cancer presents unique symptoms, but some of the most common symptoms are:
- Coughing/chest pain
- Frequent infections
- Fever or chills
- Unexplained rash/bruising/bleeding
- Loss of appetite/nausea
- Night sweats
- Persistent weakness/fatigue
- Shortness of breath
- Swollen, painless lymph nodes
Risk Factors:
Although blood cancer’s causes are not fully understood, there are risk factors for development:
- Family History: Some forms of cancer can be caused by inherited genetic mutations.
- Smoking: Smoking can cause cancer almost anywhere in the body, including the blood.
- Radiation/Chemical Exposure: Exposure to certain chemicals or cancer radiation can also increase risk for developing a form of the disease.
- Viral Exposure: HIV, Epstein-Barr virus, and human T-cell lymphoma/leukemia virus can also increase the risk for developing leukemia or lymphoma.
Treatment:
Doctors will treat blood cancer based on the type, stage, genetics, blood cell counts, overall health and specific symptoms. However, there are some common forms of treatment.
- Chemotherapy – Drugs to treat the cancer.
- Immunotherapy – Utilize natural immune system defenses.
- Radiation – High frequency waves to kill cancer cells.
- Stem Cell Bone Marrow Transplantation – Full replacement of cells that can grow into healthy blood cells.
If you or anybody you know may be affected by blood cancer, please contact your physician to seek a professional opinion.